The Complete Guide to Remote Patient Monitoring
- May 26, 2021
- Posted by: Dr Vinati Kamani
- Category: Telemedicine App Development
The use of telemedicine technology to enable the monitoring of patients outside of the conventional clinical settings has been around for quite some time now.
The first documented use of remote patient monitoring technology was back in the 1970s when Kaiser Foundation International partnered up with Lockheed Missiles and Space Company to create a remote monitoring system capable of providing healthcare delivery to rural locations without many medical services.
However, the technology remained in a nascent stage until very recently. The full potential of RPM and its associated technologies is truly being felt in the wake of the COVID-19 pandemic. As the need for innovative digital health technologies increased, remote patient monitoring has been gaining traction along with telemedicine.
A recent study of 100 clinical informatics and health IT thought leaders found that 88 percent of providers surveyed have either invested or are evaluating investments in RPM technologies.
With the healthcare industry witnessing a paradigm shift in the usage of innovative technologies for healthcare delivery, here’s the complete guide to remote patient monitoring and how you can make the most when incorporating it within your care delivery plan.
What is remote patient monitoring and how is it different from telehealth?
Centre for Connected Health Policy (CCHP) defines Remote Patient Monitoring as the personal health and medical data collection from an individual in one location, which is transmitted via electronic communication technologies to a provider in a different location for use in care and related support.
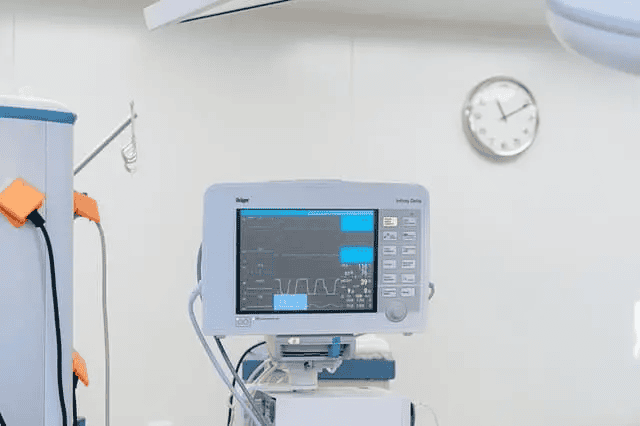
Remote patient monitoring is a subset of telehealth that uses technology tools to track patient data outside the standard healthcare settings. The software, hardware, and digital connection that capture and transmit the data through the Internet are key to at-home monitoring of patients through RPM technology.
Remote patient monitoring makes use of medical devices and healthcare wearables to collect patient data and transmit it over to the consulting physician. This technology helps physicians deliver care out of the conventional hospital-based care scenarios using the patient data and vitals that the devices send over.
Both remote patient monitoring and telemedicine are subsets of telehealth. A patient exhibiting symptoms of COVID-19 and seeking virtual consultations with a healthcare provider is a form of telemedicine.
Whereas, healthcare practitioners using data collected from connected devices such as digital thermometers, pulse oximeters, etc. to determine the treatment protocol and modify it on a real-time basis depending on patient data falls under remote patient monitoring. However, both these forms of healthcare delivery fall under the broad category of telehealth.
Benefits of Remote Patient Monitoring
1. Continuous monitoring of patients
Remote patient monitoring allows healthcare providers to have access to a continuous stream of data collected by the connected devices. RPM devices can collect a wide range of health data from the point of care, including patient weight, blood pressure, temperature, pulse rate, blood sugar levels, blood oxygen levels, heart rate, and electrocardiograms.
When the data signals an area of concern that requires the attention of the treating physician, a red flag is raised and immediate care is delivered.
Continuous monitoring of the patients also allows the care providers to make data-driven decisions and change the treatment protocol and alter prescriptions using real-time patient data for decision making. For instance, one of the recent applications of remote patient monitoring can be found in GLP-1 virtual clinics. Integration of RPM in GLP-1 virtual clinic allows providers to keep a track of patient weight and recommend GLP-1 drugs for weight loss.
2. Boosting quality of care
RPM is an effective way to ensure all patients are able to receive quality, continuous care and shift from a fee-for-service model to a value-based care one.
Using patient data as a basis for medical decision-making has proven to be helpful in reducing the number of hospitalizations, lessening the instances of readmission and bringing down the length of stay in the hospitals. This in turn is ramping up the quality of care that the patients receive.
3. Increasing patient engagement
Remote monitoring tools have proven to be effective at eliminating wait times and improving the speed of care delivery, thus boosting patient engagement levels.
By making patients an active participant in their healthcare regimen, RPM technology aims to overhaul the existing patient engagement landscape and make individuals stakeholders in their own health.
4. Improving the access to care
Remote patient monitoring in combination with telemedicine is helping care providers to overcome barriers that exist for access to care. RPM technology has made it possible for patients living in remote or rural areas to get access to the best care.
RPM is also a boon for patients who are suffering from chronic conditions, people with disabilities, as well as elderly patients who cannot make frequent trips down to the hospital for their checkups.
By having a frequent and comprehensive view of the vital signs associated with a patient’s chronic conditions such as COPD, hypertension, congestive heart failure, and diabetes, healthcare providers can formulate better care plans.
It also allows for the planning of real-time interventions, preventing the patient’s condition from worsening further by providing timely care.
Considerations when incorporating remote patient monitoring in care delivery pathways
Remote patient monitoring has numerous benefits for patients as well as healthcare providers. However, certain considerations need to be paid attention to when implementing innovative technologies into the care delivery pathways.
1. Ensure adherence to HIPAA
Healthcare data is a form of protected health information (PHI). The HIPAA privacy and security rule lays out the best practices that healthcare providers and their business associates need to follow to ensure the protection of sensitive health information.
The safety and security of healthcare data whether in storage or in transit need to be accounted for and the data collected by healthcare wearables and connected medical devices is no exception. Adequate protective measures need to be in place to safeguard patient data that is being collected, stored or transmitted for staying compliant with HIPAA norms.
2. Plan for remuneration
In the wake of the pandemic, HHS and CMS released an interim final rule that gave providers more flexibility to furnish services using remote care technology for the duration of the public health emergency. It also specified that healthcare providers could utilize remote patient monitoring for the treatment of acute and chronic conditions.
However, a plan for reimbursement of remote patient monitoring services provided needs to be in place. A remuneration plan charts out a path for RPM technology to remain viable while accounting for the operational costs associated with the technology.
3. Partner with the specialists
When you are planning to incorporate remote patient monitoring and telemedicine in your hospital workflow, partnering with the right sources can help you get started on the right note.
A dedicated healthcare software development company is already well-versed in the stringent requirements in place when developing tech solutions for healthcare providers.
Whether it is ensuring compliance with HIPAA norms in the development phase or planning for HIPAA compliant storage of patient data, specialists in the healthcare field already know what the best practices are, thereby increasing the chances of your success.
Closing words
Remote patient monitoring brings in the premise of using the power of early interventions to improve overall health outcomes. Proper planning and implementation of technology can help you spearhead innovation, improve patient satisfaction and streamline care while cutting down on the associated healthcare costs.
Thinking of incorporating remote patient monitoring and telemedicine in your healthcare delivery workflow? Get in touch with our expert consultants and get the answers to all your technology-related queries.
