How to Start a Telehealth Business: 2026 Guide
- January 13, 2026
- Posted by: Dr Vinati Kamani
- Category: Telemedicine App Development
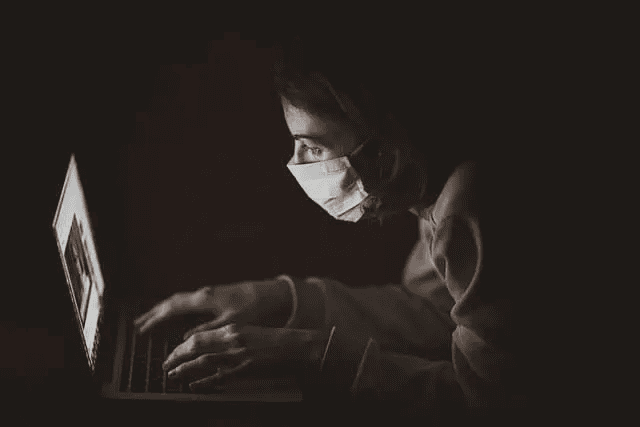
The telehealth industry has experienced unprecedented growth, creating massive opportunities for entrepreneurs and healthcare professionals. With patient expectations evolving and technology advancing rapidly, now represents an ideal time to launch a successful telehealth business.
Recent surveys reveal that 53% of patients abandon scheduled appointments due to excessive wait times, while 71% expressed concerns about visiting healthcare facilities during health crises. These statistics highlight the significant market demand driving telehealth adoption across the United States.
Ready to Launch Your Telehealth Platform? Arkenea brings 14+ years of exclusive healthcare software expertise, as an asynchronous and synchronous telemedicine app development company, to help you build a custom telehealth solution that meets your unique business requirements. Schedule your free consultation to discuss your vision.
Table of Contents
- Market Opportunity & Growth Potential
- Business Model Selection & Revenue Streams
- Target Market Analysis & Patient Segmentation
- Technology Architecture Planning
- Regulatory Compliance & Legal Framework
- Financial Planning & Investment Analysis
- 15 Essential Steps to Launch Your Telehealth Business
- Marketing Strategy & Patient Acquisition
- Advanced Security Framework
- Operational Excellence & Quality Management
- Growth & Scaling Strategies
- Choosing the Right Technology Partner
Core Telehealth Service Categories
Virtual Consultations represent the most common telehealth service, enabling patients to connect with healthcare providers through secure video or audio platforms. These appointments eliminate geographical barriers and reduce patient travel time while maintaining clinical effectiveness.
Remote Patient Monitoring involves collecting patient health data through connected devices and sensors, allowing providers to track chronic conditions, medication adherence, and recovery progress between visits.
Store and Forward Technologies enable asynchronous communication where patients submit medical information, images, or test results for later review by healthcare professionals. This approach particularly benefits specialties like dermatology and pathology.
Digital Therapeutics provide evidence-based therapeutic interventions delivered through software applications, offering treatment for conditions ranging from mental health disorders to chronic disease management.
Telehealth Market Opportunity and Growth Potential
The telehealth market presents extraordinary growth opportunities driven by demographic shifts, technology adoption, and evolving healthcare needs. Understanding these market dynamics will inform your strategic planning and investment decisions.
Industry Growth Metrics
The global telehealth market reached $83.5 billion in 2022 and projects to grow at a compound annual growth rate of 24.3% through 2030. This expansion reflects increasing consumer acceptance, regulatory support, and healthcare cost pressures driving adoption across all patient demographics.
Millennial patients show particularly strong preferences for digital health solutions, with 40% expressing interest in telehealth services compared to 28% of Generation X patients. This demographic shift indicates sustained long-term growth potential for telehealth businesses.
Geographic Market Variations
Rural markets present significant opportunities due to physician shortages and limited healthcare access. Approximately 20% of Americans live in rural areas where specialist availability remains severely constrained, creating natural market demand for telehealth services.
Urban markets offer different advantages, including higher technology adoption rates, better internet infrastructure, and greater willingness to pay for convenience-focused healthcare services.
How To Start A Telehealth Business: A Comprehensive Guide
As the telehealth industry continues to grow rapidly, starting a telehealth business today is an exciting opportunity for both entrepreneurs and healthcare professionals. Advances in technology and changing patient expectations, accelerated by concerns around visiting healthcare facilities in person, have driven a strong shift toward virtual care.
This comprehensive guide from Arkenea, with more than 14 years of experience in healthcare software development, will walk you through the key steps to launch and scale a successful telehealth platform, from shaping your business model and ensuring compliance to streamlining operations and choosing the right technology partner.
Telehealth Business Model Selection and Revenue Streams
Selecting the appropriate business model determines your target customers, revenue potential, and operational complexity. Each model offers distinct advantages and challenges that align with different entrepreneurial goals and market opportunities.
Direct-to-Consumer (B2C) Telehealth Model
B2C telehealth businesses serve individual patients directly, typically through subscription services or fee-per-visit arrangements. This model offers higher profit margins and direct customer relationships but requires significant marketing investment and patient acquisition efforts.
Successful B2C examples include mental health platforms, urgent care services, and specialized wellness programs. Revenue streams include membership fees, consultation charges, prescription fulfillment margins, and premium service tiers.
Business-to-Business (B2B) Telehealth Model
B2B telehealth companies provide services to healthcare organizations, employers, or insurance companies. This model typically generates more predictable revenue through enterprise contracts but involves longer sales cycles and complex procurement processes.
B2B opportunities include white-label platforms for healthcare systems, employee wellness programs for corporations, and specialized services for insurance companies seeking to reduce medical costs.
Hybrid B2B2C Telehealth Approach
Many successful telehealth companies combine B2B and B2C elements, partnering with organizations to reach end consumers. This approach leverages institutional credibility while accessing larger patient populations through existing healthcare relationships.
Revenue Stream Diversification
Mature telehealth businesses typically develop multiple revenue streams including consultation fees, subscription services, medication fulfillment, diagnostic testing partnerships, and premium features. This diversification reduces dependence on single revenue sources and improves financial stability.
Telehealth Target Market Analysis & Patient Segmentation
Successful telehealth businesses begin with precise target market identification and patient segmentation. This strategic foundation influences everything from technology development to marketing messaging and service delivery approaches.
Demographic Segmentation
Age demographics significantly impact telehealth adoption patterns and service preferences. Younger patients (ages 25-45) typically prefer mobile-first solutions with streamlined interfaces, while older populations may require additional support and prefer video-based consultations over text-based interactions.
Geographic considerations include urban professionals seeking convenience, suburban families managing multiple schedules, and rural patients requiring specialist access. Each segment presents different value propositions and service delivery requirements.
Clinical Specialty Focus
Specializing in specific medical areas allows for deeper expertise development and targeted marketing efforts. High-opportunity specialties include mental health services, dermatology consultations, chronic disease management, and urgent care visits.
Mental health represents particularly strong growth potential, with telehealth visits for behavioral health increasing 3800% during peak adoption periods. This specialty benefits from reduced stigma associated with virtual visits and strong clinical outcomes data.
Psychographic and Behavioral Factors
Patient motivations for seeking telehealth services include convenience preferences, privacy concerns, mobility limitations, time constraints, and cost considerations. Understanding these underlying drivers enables more effective service positioning and marketing messaging.
Technology comfort levels vary significantly across patient populations, requiring different onboarding approaches and support resources. Some patients need extensive guidance while others prefer self-service options with minimal intervention.
Technology Architecture Planning for Telehealth Business
Technology architecture decisions form the foundation of your telehealth business, impacting scalability, security, user experience, and operational efficiency. These choices require careful consideration of current needs and future growth plans.
Platform Development Approaches
Custom software development offers maximum flexibility and competitive differentiation but requires significant upfront investment and longer development timelines. This approach works best for businesses with unique workflow requirements or specialized clinical needs.
Software-as-a-Service (SaaS) platforms provide faster market entry and lower initial costs but limit customization options and create ongoing dependency on third-party providers. Many successful telehealth businesses begin with SaaS solutions before transitioning to custom platforms as they scale.
Core Technology Components
Video conferencing capabilities require high-quality, low-latency solutions that work reliably across different devices and network conditions. Consider WebRTC-based solutions for browser compatibility or native mobile applications for enhanced performance.
Electronic Health Record (EHR) integration enables seamless clinical workflows and reduces duplicate data entry. Popular integration standards include HL7 FHIR, which facilitates interoperability between different healthcare systems.
Patient scheduling and appointment management systems should include automated reminders, rescheduling capabilities, and integration with provider calendars. These features significantly impact patient satisfaction and operational efficiency.
Scalability and Performance Considerations
Cloud infrastructure provides the flexibility needed to handle varying demand patterns while maintaining cost efficiency. Consider multi-region deployment to reduce latency and improve user experience across different geographic areas.
Database architecture must accommodate healthcare data requirements including audit trails, data retention policies, and high availability needs. Consider both relational databases for structured clinical data and NoSQL solutions for unstructured content.
Mobile Application Strategy
Native mobile applications typically provide superior user experiences compared to web-based solutions, particularly for video consultations and real-time communication features. However, they require additional development resources and ongoing maintenance across multiple platforms.
Progressive Web Applications (PWAs) offer a middle ground, providing app-like experiences through web browsers while reducing development complexity and maintenance overhead.
Telehealth Regulatory Compliance & Legal Framework
Healthcare regulations create complex compliance requirements that vary by location, specialty, and business model. Understanding these frameworks prevents costly violations and builds patient trust in your services.
HIPAA Compliance Requirements
The Health Insurance Portability and Accountability Act (HIPAA) establishes comprehensive privacy and security standards for protected health information (PHI). Compliance requirements include administrative, physical, and technical safeguards that must be implemented throughout your technology infrastructure.
Business Associate Agreements (BAAs) must be signed with all third-party vendors who may access PHI, including cloud hosting providers, payment processors, and software vendors. These agreements establish legal responsibility for PHI protection across your vendor relationships.
Data encryption requirements mandate both data at rest and data in transit protection using industry-standard encryption methods. This includes database encryption, secure file storage, and encrypted communication channels for all patient interactions.
State Licensing and Practice Requirements
Healthcare provider licensing remains primarily state-based, creating complex requirements for multi-state telehealth operations. Most states require providers to hold active licenses in states where patients are located during consultations.
Interstate Medical Licensure Compact provides streamlined licensing processes for qualified physicians, currently including 32 participating states. This program significantly reduces administrative burden for providers seeking multi-state practice authority.
Prescribing regulations vary significantly by state, particularly for controlled substances. The DEA requires special registration for telemedicine prescribing, and some states impose additional restrictions on remote prescribing practices.
FDA and Medical Device Regulations
Software applications that provide diagnostic recommendations or treatment guidance may require FDA approval as medical devices. Understanding these requirements early in development prevents costly delays or compliance violations.
Remote monitoring devices and diagnostic tools often require FDA clearance before commercial use. Partner with established device manufacturers to leverage existing approvals rather than pursuing independent device development.
Financial Planning & Investment Analysis for Starting a Telehealth Business
Comprehensive financial planning enables informed decision-making about funding requirements, pricing strategies, and growth investments. These projections also support fundraising efforts and investor discussions.
Startup Cost Analysis
Technology development represents the largest initial investment for most telehealth businesses. Custom platform development typically ranges from $150,000 to $500,000 depending on feature complexity and integration requirements.
Regulatory compliance costs include legal consulting, security audits, and ongoing compliance monitoring. Budget approximately $25,000 to $75,000 for initial compliance setup and $10,000 to $30,000 annually for ongoing compliance maintenance.
Professional licensing fees vary by state but typically range from $500 to $2,000 per state for physician licenses. Malpractice insurance costs approximately $8,000 to $24,000 annually depending on specialty and coverage limits.
Revenue Projections and Modeling
Patient acquisition costs in telehealth typically range from $50 to $200 per patient depending on marketing channels and service types. Digital marketing generally provides more cost-effective acquisition compared to traditional healthcare marketing approaches.
Average revenue per patient varies significantly by specialty and service model. Mental health services often generate $100 to $200 per session, while urgent care consultations typically range from $40 to $80 per visit.
Patient retention rates directly impact long-term profitability. Successful telehealth businesses achieve 70% to 85% patient retention rates through quality care delivery and positive user experiences.
Return on Investment (ROI) Calculations
Break-even analysis should consider both fixed costs (technology, compliance, overhead) and variable costs (provider payments, payment processing, marketing). Most telehealth businesses achieve break-even within 18 to 36 months with proper execution.
Customer lifetime value calculations help justify marketing investments and pricing decisions. Consider both direct revenue from consultations and indirect revenue from referrals and additional services.
Funding Options and Requirements
Bootstrap funding works well for simple telehealth businesses with limited technology requirements and local market focus. This approach maintains control but limits growth speed and market expansion capabilities.
Venture capital funding enables rapid scaling and market expansion but requires significant equity sacrifice and growth pressure. Healthcare-focused investors bring valuable industry expertise alongside capital investment.
Revenue-based financing provides growth capital without equity dilution, making it attractive for profitable telehealth businesses seeking expansion funding.
15 Essential Steps to Launch Your Telehealth Business
These actionable steps provide a structured approach to launching your telehealth business while ensuring compliance and market readiness. Each step builds upon previous work to create a comprehensive foundation for success.
1. Medical Certification and Credentialing
Healthcare provider certification requirements vary by state and specialty but generally require completion of accredited medical education programs and passing relevant board examinations. Contact your state medical board to understand specific requirements for your intended practice area.
Physician credentialing with hospitals and healthcare systems can take 90 to 180 days to complete. Begin this process early since credentialing often requires active practice history and reference verification from multiple sources.
2. State Licensing and Registration
Medical license applications typically require 6 to 12 months for processing, though some states offer expedited licensing for qualified applicants. Research Interstate Medical Licensure Compact participation if you plan multi-state operations.
Temporary licensing options became more common during the pandemic, with some states offering 30-day temporary licenses for qualified practitioners. These options can accelerate market entry while permanent licenses process.
3. National Provider Identifier (NPI) Registration
The National Provider Identifier provides a unique 10-digit identification number for healthcare providers participating in standard transactions. Apply through the National Plan and Provider Enumeration System (NPPES) website at no cost.
NPI numbers typically process within 7 to 10 business days for online applications. This identifier is required for insurance billing, Medicare enrollment, and most healthcare transactions.
4. Employer Identification Number (EIN) Application
The Internal Revenue Service issues EIN numbers for business tax identification purposes. Apply online, by phone, or by mail through the IRS website. Online applications receive immediate EIN assignment during business hours.
EIN numbers are required for business bank accounts, employee payroll, and tax filing purposes. Solo practitioners may use Social Security Numbers instead of EIN numbers for some purposes.
5. Business Structure and Legal Entity Formation
Limited Liability Company (LLC) structures provide operational flexibility and personal liability protection for most telehealth businesses. Professional LLCs may be required in some states for healthcare practices.
Corporate structures offer additional benefits for businesses seeking venture capital investment or planning public offerings. Consult with healthcare attorneys to select optimal business structures for your specific situation.
6. Professional Workspace Setup
Physical office space requirements vary by state and practice type. Many telehealth businesses operate successfully with home-based offices or shared workspace arrangements that reduce overhead costs.
Professional workspace design should consider patient privacy, lighting quality, and background appearance for video consultations. Invest in quality audio and video equipment to ensure professional presentation during patient interactions.
7. Business Banking and Financial Management
Business bank accounts separate personal and professional finances while building business credit history. Many banks offer specialized healthcare practice banking services with features designed for medical practices.
Merchant services for credit card processing should include healthcare-specific features like HIPAA-compliant payment processing and integration with practice management systems. Compare processing fees across multiple providers to optimize costs.
8. Malpractice Insurance Coverage
Professional liability insurance protects against malpractice claims and regulatory violations. Telemedicine-specific coverage addresses unique risks associated with remote care delivery and technology failures.
Occurrence-based policies provide longer-term protection compared to claims-made policies, though they typically cost 20% to 30% more. Consider coverage limits based on your specialty and state requirements.
9. DEA Registration for Prescribing Authority
Drug Enforcement Administration registration enables controlled substance prescribing authority. Apply through the DEA website with supporting documentation including medical licenses and practice information.
Telemedicine prescribing regulations vary by state and substance classification. Some controlled substances cannot be prescribed through telemedicine without prior in-person examinations.
10. Medicare and Insurance Enrollment
Medicare enrollment enables billing for telehealth services covered under Medicare programs. The application process typically requires 90 to 120 days for completion and requires active medical licensing.
Commercial insurance credentialing varies by payer but generally requires similar documentation to Medicare enrollment. Consider using credentialing services to streamline applications across multiple insurance companies.
11. HIPAA-Compliant Technology Platform
Technology platform selection significantly impacts patient experience, operational efficiency, and compliance requirements. Evaluate platforms based on video quality, ease of use, integration capabilities, and security features.
Custom development provides maximum flexibility but requires significant investment and development time. SaaS platforms offer faster deployment but may limit customization options and create ongoing subscription costs.
12. Medical Billing and Revenue Cycle Management
Medical billing for telehealth services requires understanding of telemedicine-specific billing codes and documentation requirements. Consider outsourcing billing functions initially to focus on patient care and business development.
Revenue cycle management includes patient eligibility verification, prior authorization processing, claims submission, and denial management. Efficient billing processes directly impact cash flow and profitability.
13. Quality Assurance and Clinical Protocols
Clinical protocols ensure consistent care delivery and regulatory compliance across all patient interactions. Develop standardized procedures for patient screening, consultation documentation, and follow-up care coordination.
Quality metrics should include patient satisfaction scores, clinical outcome measures, and operational efficiency indicators. Regular quality reviews identify improvement opportunities and ensure optimal patient care.
14. Staff Training and Workflow Integration
Team training ensures smooth technology adoption and consistent patient experiences. Include technical troubleshooting, customer service skills, and emergency procedure protocols in training programs.
Workflow integration requires coordination between clinical staff, administrative personnel, and technology systems. Document all procedures to ensure consistent execution and facilitate staff onboarding.
15. Data Security and Privacy Framework
Comprehensive security frameworks protect patient information and ensure regulatory compliance. Include technical safeguards (encryption, access controls), administrative safeguards (policies, training), and physical safeguards (facility security, device management).
Regular security audits identify vulnerabilities and ensure ongoing compliance with evolving regulations. Consider third-party security assessments to validate your protection measures.
Marketing Strategy & Patient Acquisition
Effective marketing strategies combine digital channels, professional networking, and community outreach to build patient awareness and drive sustainable growth. Healthcare marketing requires careful attention to compliance and professional standards.
Digital Marketing Foundations
Search engine optimization (SEO) drives organic traffic by improving visibility for relevant healthcare searches. Focus on local SEO for location-based services and condition-specific content for specialized practices.
Content marketing establishes expertise and builds patient trust through educational resources. Blog posts, video content, and social media presence demonstrate knowledge while providing value to potential patients.
Pay-per-click (PPC) advertising provides immediate visibility but requires careful budget management and compliance with healthcare advertising regulations. Google Ads and social media advertising offer precise targeting options for healthcare practices.
Professional Network Development
Physician referral relationships remain crucial for specialty telehealth services. Develop relationships with primary care providers, hospitals, and complementary specialists who can refer appropriate patients.
Professional organization participation builds credibility and provides networking opportunities. Consider joining telemedicine associations, medical societies, and local business organizations relevant to your practice area.
Patient Retention and Satisfaction
Patient experience optimization includes streamlined scheduling, clear communication, and follow-up care coordination. Small improvements in user experience significantly impact patient satisfaction and retention rates.
Patient feedback systems provide insights for continuous improvement while demonstrating commitment to quality care. Regular surveys and review monitoring help identify areas for enhancement.
Advanced Security Framework
Healthcare cybersecurity requires comprehensive protection strategies that address evolving threats while maintaining regulatory compliance. Security breaches can destroy patient trust and result in significant financial penalties.
Data Encryption and Protection
End-to-end encryption protects patient communications during transmission between devices and servers. Implement AES-256 encryption standards for stored data and TLS 1.3 for data transmission.
Database security includes role-based access controls, audit logging, and regular backup procedures with tested recovery processes. Consider database encryption for additional protection of sensitive patient information.
Access Control and Authentication
Multi-factor authentication (MFA) adds security layers beyond simple passwords. Require MFA for all system access, including administrative functions and clinical applications.
Role-based permissions ensure users access only information necessary for their job functions. Regular access reviews identify unused accounts and inappropriate permission levels.
Incident Response and Disaster Recovery
Security incident response plans outline procedures for identifying, containing, and recovering from security breaches. Include notification procedures for patients, regulators, and law enforcement as required.
Disaster recovery planning ensures business continuity during technology failures or security incidents. Test recovery procedures regularly to ensure effectiveness when needed.
Operational Excellence & Quality Management
Operational excellence creates sustainable competitive advantages through efficient processes, consistent quality, and exceptional patient experiences. These foundations support long-term business success and growth.
Clinical Quality Standards
Evidence-based care protocols ensure consistent treatment approaches and optimal patient outcomes. Develop specialty-specific guidelines that incorporate telehealth best practices and regulatory requirements.
Clinical documentation standards maintain compliance while supporting quality improvement initiatives. Standardized templates reduce documentation time while ensuring comprehensive record-keeping.
Performance Measurement and Analytics
Key performance indicators (KPIs) should include patient satisfaction scores, clinical outcome measures, operational efficiency metrics, and financial performance indicators. Regular reporting enables data-driven decision making.
Analytics platforms provide insights into patient behavior, system usage patterns, and operational bottlenecks. Use this data to optimize workflows and improve patient experiences.
Continuous Improvement Processes
Quality improvement methodologies like Plan-Do-Study-Act (PDSA) cycles provide structured approaches to operational enhancement. Focus improvements on areas with greatest impact on patient satisfaction and business performance.
Staff feedback systems capture operational insights from team members who interact directly with patients and technology systems. Front-line staff often identify improvement opportunities that management might miss.
Growth & Scaling Strategies
Sustainable growth requires strategic planning around market expansion, service diversification, and operational scaling. These decisions significantly impact resource requirements and long-term success potential.
Market Expansion Planning
Geographic expansion requires understanding of state-specific regulations, licensing requirements, and market conditions. Prioritize states with favorable telehealth regulations and underserved patient populations.
Service line expansion can leverage existing patient relationships while diversifying revenue streams. Consider complementary services that align with your clinical expertise and patient needs.
Technology Scaling and Integration
Platform architecture must accommodate growth in user volume, feature complexity, and integration requirements. Plan technology infrastructure to handle 10x current usage without major architectural changes.
Third-party integrations with EHR systems, billing platforms, and diagnostic services improve operational efficiency while enhancing patient experiences. Prioritize integrations that eliminate duplicate data entry or streamline workflows.
Partnership and Acquisition Opportunities
Strategic partnerships with healthcare systems, insurance companies, or technology vendors can accelerate growth while providing access to new markets and capabilities.
Acquisition opportunities may include complementary telehealth businesses, specialized technology platforms, or established patient populations. Evaluate opportunities based on strategic fit and financial returns.
Choosing the Right Technology Partner
Your technology development partner significantly impacts project success, timeline, and long-term operational capabilities. Healthcare software development requires specialized expertise that goes beyond general software development skills.
Healthcare Industry Experience
Healthcare-specific development experience includes understanding of clinical workflows, regulatory requirements, and user experience considerations unique to medical practices. Look for partners with healthcare software portfolios and relevant case studies.
Regulatory compliance expertise prevents costly mistakes and ensures proper implementation of HIPAA, FDA, and state-specific requirements. Partners should demonstrate knowledge of healthcare regulations and compliance frameworks.
Technical Capabilities and Architecture
Full-stack development capabilities enable comprehensive platform development without requiring multiple vendor relationships. Look for expertise in both front-end user experience design and back-end infrastructure development.
Integration experience with healthcare systems, billing platforms, and third-party services accelerates development timelines while reducing technical risks. Ask for specific examples of healthcare system integrations.
Support and Maintenance Considerations
Post-launch support includes bug fixes, security updates, feature enhancements, and technical support services. Understand support availability, response times, and cost structures before making development commitments.
Scalability planning ensures your platform can handle growth in users, transaction volume, and feature complexity. Discuss architecture approaches for handling increased usage without performance degradation.
Why Arkenea Is Your Ideal Telehealth Development Partner
Arkenea brings 14+ years of exclusive healthcare software development experience, having successfully delivered custom telehealth platforms for medical practices, healthcare systems, and digital health startups across multiple specialties.
Our healthcare-focused expertise includes comprehensive HIPAA compliance implementation, clinical workflow optimization, and integration with popular EHR systems like Epic, Cerner, and Allscripts. We understand the unique challenges of healthcare technology development.
Our custom development approach ensures your telehealth platform perfectly matches your clinical workflows and business requirements rather than forcing adaptation to generic solutions. Every feature serves your specific practice needs and patient populations.
From initial consultation through post-launch support, Arkenea provides comprehensive partnership that includes strategic planning, technical architecture, regulatory compliance, and ongoing maintenance services. We invest in your long-term success.
Ready to Transform Healthcare Delivery?
Partner with Arkenea, 14+ years of experience as a telemedicine app development company, to help you develop a custom telehealth platform that differentiates your practice and delivers exceptional patient experiences. Our healthcare technology experts will guide you through every step of the development process.
