Medical Device Integration: 2025’s Complete Guide
- June 18, 2025
- Posted by: Rahul Varshneya
- Category: Healthcare Technology
In today’s rapidly evolving healthcare landscape, medical device integration stands at the forefront of innovation, connecting disparate devices, systems, and data sources to deliver seamless, real-time insights.
From intensive care units to remote patient monitoring, integrating medical devices into electronic health record (EHR) and electronic medical record (EMR) platforms is no longer optional, it’s essential for improving patient outcomes, streamlining clinical workflows, and ensuring data based decision making.
Introduction to Medical Device Integration
What is Medical Device Integration?
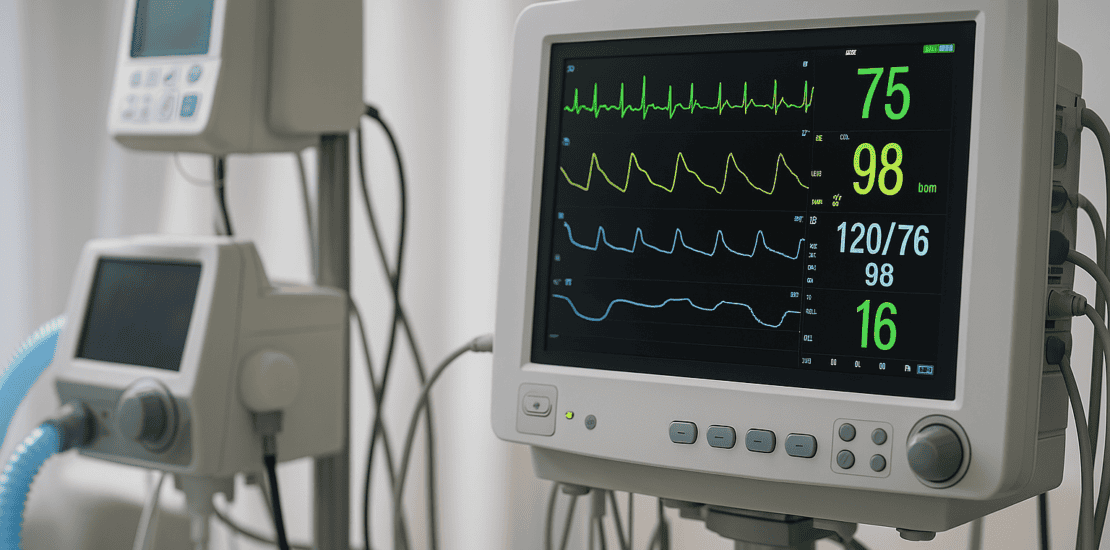
Medical device integration refers to the process of connecting clinical devices such as patient monitors, infusion pumps, ventilators, imaging systems, and wearable sensors, to hospital information systems, EHR/EMR platforms, and other software applications. By enabling bi-directional, real time data exchange, integration transforms isolated devices into a unified ecosystem of connected medical devices, fostering greater situational awareness and operational efficiency.
Why It Matters
- Enhanced Patient Care: Continuous, accurate data from integrated devices empowers clinicians to detect early warning signs, adjust treatments on the fly, and deliver personalized care plans.
- Streamlined Workflows: Automated data capture eliminates manual charting, reduces transcription errors, and frees up staff to focus on patient-facing activities.
- Interoperability & Collaboration: Seamless sharing of device data across departments like ICU, radiology, cardiology, telehealth, supports multidisciplinary care teams and improves care coordination.
In an era where healthcare providers must do more with less, medical device integration delivers the technological backbone necessary to optimize clinical operations, bolster patient safety, and meet regulatory requirements around data security and privacy.
Arkenea has 14+ years of experience as a custom healthcare software development company to help bring your healthcare project to life. Get in touch for a free consultation.
Benefits of Medical Device Integration
2.1 Improved Patient Outcomes Through Integration
When patient monitors, infusion pumps, and wearable sensors feed data directly into the EHR, clinicians gain a holistic, real time view of vital signs, medication administration, and activity levels.
- Early Detection of Deterioration: Automated alerts for changes in heart rate, oxygen saturation, or blood pressure can trigger rapid interventions, reducing ICU transfers and adverse events.
- Data-Driven Decisions: Access to longitudinal device data supports trend analysis, enabling evidence-based adjustments to treatment protocols.
- Personalized Care Plans: Insights from integrated devices guide tailored therapies from titrating ventilator settings to adjusting insulin doses based on each patient’s unique physiological response.
2.2 Enhanced Workflow Efficiency
Manual data entry is labor intensive and prone to errors. Medical device integration automates this process, resulting in:
- Reduced Charting Time: Nurses and technicians spend less time transcribing readings, allowing more time for direct patient care.
- Fewer Documentation Errors: Automated transfer of device outputs to the EHR virtually eliminates transcription mistakes that can lead to misdiagnoses or medication errors.
- Streamlined Rounds and Reporting: Clinicians access consolidated dashboards showing device metrics alongside lab results and physician notes, accelerating rounds and multidisciplinary discussions.
Efficient workflows translate to cost savings, higher staff morale, and more consistent compliance with documentation standards.
2.3 Better Patient Safety with Automated Alerts
Integration platforms can be configured to generate automated alarms and clinical decision support (CDS) notifications based on predefined thresholds.
- Critical Event Notifications: Real time alerts for arrhythmias, hypoxia, or infusion pump occlusions ensure rapid clinical responses.
- Closed Loop Medication Management: Integration between infusion pumps and pharmacy systems reduces wrong-dose or wrong drug errors.
- Device Malfunction Detection: Continuous health checks on connected devices flag calibration issues or connectivity losses before they compromise patient safety.
Key Components of Medical Device Integration
3.1 Hardware: The Foundation of Connectivity
At the device level, integration begins with physical connections and data capture modules:
- Patient Monitoring Devices: Bedside monitors for ECG, SpO₂, NIBP, and temperature equipped with network interfaces.
- Infusion Pumps and Ventilators: Smart pumps and ventilators capable of exporting dosage rates and respiratory parameters.
- Imaging Equipment: CT, MRI, and ultrasound systems that generate DICOM images and metadata.
- Wearables and IoMT Sensors: Bluetooth or Wi-Fi enabled devices tracking mobility, hydration, glucose levels, and more.
Modern devices often support standard communication protocols (e.g., IEEE 11073, HL7 v2/v3) and can be retrofitted with network gateways to connect legacy equipment.
3.2 Software: Middleware and EHR/EMR Integration
Software forms the bridge between device outputs and clinical systems:
- Middleware Platforms: Specialized integration engines that normalize device data, manage device connectivity, and orchestrate data routing.
- HL7/FHIR Interfaces: Adapters that transform device data into HL7 messages or FHIR resources for consumption by EHRs, analytics tools, and CDS modules.
- EHR/EMR Systems: Central repositories where patient records, device streams, lab results, and physician documentation converge.
- Analytics Dashboards: Visualization tools and reporting engines that aggregate device metrics for clinical and operational insights.
A robust middleware layer ensures scalability, high availability, and support for new device types and standards as technology evolves.
3.3 Security: Protecting Patient Data
Given the sensitivity of health information, security is paramount:
- HIPAA Compliance: Ensuring all data exchanges meet the Health Insurance Portability and Accountability Act requirements for privacy and security.
- Data Encryption: TLS/SSL for data in transit, AES 256 for data at rest, and end-to-end encryption for wireless device communications.
- Access Controls & Auditing: Role-based access, multi-factor authentication, and comprehensive audit logs to track who accessed or modified device data.
- Network Segmentation: Isolating medical device traffic from general IT networks to reduce attack surfaces and contain potential breaches.
By embedding security at every layer from device firmware to cloud storage, organizations can maintain patient trust and avoid costly compliance violations.
Challenges in Medical Device Integration
4.1 Technical Barriers & Lack of Standardization
- Proprietary Protocols: Many devices use vendor specific communication formats, requiring custom adapters or reverse engineering.
- Legacy Equipment: Older devices may lack network interfaces, forcing hospitals to deploy physical gateways or manual workarounds.
- Fragmented Standards: Multiple standards (IEEE 11073, HL7 v2/v3, DICOM, FHIR) coexist, and mapping between them can be complex and error prone.
4.2 Regulatory Compliance & Certification
- FDA Oversight: Device connectivity solutions may be subject to FDA regulation as medical devices or accessories, necessitating validation, testing, and documentation.
- Data Privacy Laws: Beyond HIPAA, global organizations must navigate GDPR (EU), PIPEDA (Canada), and other regional privacy regulations.
- Clinical Validation: Integration workflows often require clinical trials or pilot programs to verify safety and efficacy before full scale deployment.
4.3 High Implementation Costs and Training Needs
- Upfront Investments: Hardware upgrades, middleware licensing, and network infrastructure can strain capital budgets.
- Ongoing Maintenance: Software updates, security patches, and device lifecycle management require dedicated IT and biomedical engineering resources.
- Staff Training: Clinicians, nurses, and IT staff must learn new workflows, interfaces, and troubleshooting procedures, which can slow adoption.
4.4 Change Management and Organizational Buy In
- Cultural Resistance: Clinicians accustomed to paper charts or manual entry may resist new digital workflows.
- Workflow Redesign: Effective integration often demands rethinking clinical processes, which can meet institutional inertia.
- Vendor Coordination: Coordinating multiple device vendors, middleware providers, and EHR partners requires strong project management and governance.
Addressing these challenges head on with a clear roadmap, stakeholder engagement, and incremental pilots can pave the way for successful integration.
Medical Device Integration Use Cases and Real World Examples
5.1 IoT Based Remote Patient Monitoring
Scenario: A home health agency monitors post-surgical patients using wearable ECG patches and Bluetooth-enabled blood pressure cuffs.
Integration Approach: Data streams from wearables feed into a cloud-based IoMT platform, which triggers alerts for arrhythmias or hypertension.
Outcome: Early detection of complications reduces hospital readmissions by 25%, improves patient satisfaction, and lowers overall costs.
5.2 Imaging Device Integration for Faster Diagnostics
Scenario: A radiology department integrates CT and MRI scanners directly with the hospital’s PACS and EHR.
Integration Approach: DICOM images and radiology reports auto-populate patient charts, and radiologists use AI-powered analytics to prioritize critical cases.
Outcome: Turnaround time for critical scans drops from 4 hours to under 60 minutes, accelerating treatment for stroke and trauma patients.
5.3 Closed Loop Medication Management
Scenario: An oncology clinic uses smart infusion pumps integrated with pharmacy systems and EHR.
Integration Approach: Oncologists order chemotherapy doses in the EHR; the middleware sends dose parameters to the infusion pump, which confirms correct drug and rate before starting.
Outcome: Zero medication errors over 18 months, enhanced compliance with safety protocols, and improved staff confidence.
5.4 ICU Central Monitoring
Scenario: A tertiary care hospital deploys a centralized monitoring station for its 50-bed ICU.
Integration Approach: Bedside monitors, ventilators, and dialysis machines stream data via middleware to a unified dashboard accessible to intensivists.
Outcome: Clinicians track multiple patients simultaneously, reducing alarm fatigue by 40% through intelligent alarm filtering and correlating device events with lab results.
Trends in Medical Device Integration
6.1 The Rise of IoMT (Internet of Medical Things)
- Ecosystem Expansion: An explosion of connected devices, from ingestible sensors to smart beds, is fueling the growth of IoMT networks.
- Edge Computing: Processing data at the device or gateway level reduces latency and preserves bandwidth for critical alerts.
- Standardization Efforts: Organizations like the Continua Health Alliance and IEEE are promoting open frameworks to ensure interoperability across IoMT devices.
6.2 Wearable Technology and Consumer Health Integration
- Patient Generated Data: Wearables (smartwatches, fitness trackers) and home medical devices (glucometers, pulse oximeters) feed data into patient portals and EHRs.
- Chronic Disease Management: Continuous glucose monitors and activity trackers enable proactive interventions for diabetes, COPD, and heart failure.
- Telehealth Synergy: Integrated wearables enhance virtual visits by providing clinicians with real-time biometric data during teleconsultations.
6.3 AI based Analytics and Predictive Insights
- Machine Learning Models: Aggregated device data trains algorithms to predict patient deterioration, sepsis onset, or risk of readmission.
- Decision Support: AI-powered CDS tools analyze device streams alongside labs and imaging to recommend interventions and optimize care pathways.
- Workflow Automation: Natural language processing (NLP) extracts key insights from unstructured device logs and clinical notes, further reducing manual work.
6.4 Cloud Native Integration and SaaS Platforms
- Scalability and Agility: Cloud hosted integration platforms reduce on premises infrastructure costs and accelerate deployment of new device connectors.
- API First Architectures: RESTful and FHIR APIs enable rapid onboarding of new devices and easy integration with third-party apps.
- Security and Compliance: Leading cloud providers offer built-in HIPAA-compliant services, encryption, and audit trails, simplifying regulatory adherence.
Best Practices for Implementing Medical Device Integration
7.1 Conduct a Comprehensive Needs Assessment
- Stakeholder Interviews: Engage clinicians, nurses, IT staff, and biomedical engineers to understand pain points and priorities.
- Device Inventory: Catalog all existing devices, communication protocols, and software versions.
- Workflow Mapping: Document current clinical processes to identify integration opportunities and potential bottlenecks.
7.2 Choose Scalable, Standards Based Solutions
- Open Standards: Prioritize platforms supporting HL7, FHIR, IEEE 11073, and DICOM to avoid vendor lock-in.
- Modular Architecture: Select middleware that allows incremental device onboarding and easy updates.
- Vendor Neutrality: Opt for vendor-agnostic solutions that integrate with multiple EHR/EMR systems and device manufacturers.
7.3 Ensure Security and Compliance from Day One
- Security by Design: Incorporate encryption, access controls, and network segmentation into your architecture blueprint.
- Regulatory Roadmap: Develop a compliance plan addressing HIPAA, FDA, GDPR, and other relevant regulations.
- Continuous Monitoring: Implement intrusion detection, vulnerability scanning, and routine audits to maintain a secure posture.
7.4 Pilot, Iterate, and Scale
- Small Scale Pilots: Start with a single department or device type to validate technical feasibility and clinical impact.
- Feedback Loops: Collect user feedback, monitor KPIs (e.g., charting time saved, alert response times), and refine workflows.
- Phased Rollout: Gradually expand integration to additional units, ensuring adequate training and support at each stage.
7.5 Invest in Training and Change Management
- Role Based Training: Provide tailored sessions for nurses, physicians, and IT personnel, focusing on hands on practice.
- Superuser Network: Identify clinical champions to serve as on-site resources and peer trainers.
- Communication Plan: Keep stakeholders informed of milestones, successes, and upcoming changes to build momentum and trust.
Conclusion
Medical device integration is a cornerstone of modern healthcare transformation. By connecting devices, systems, and data streams, providers can deliver safer, more efficient, and more personalized care. From reducing manual documentation to enabling predictive analytics, integration empowers clinicians with the insights they need to make better decisions, every minute of every day.
Next Steps:
- Assess your current state: Conduct an inventory of devices and workflows to identify integration opportunities.
- Engage experts: Partner with experienced integration vendors or consultants who understand healthcare interoperability and regulatory requirements.
- Pilot and scale: Start small, measure impact, and expand strategically to achieve organization-wide integration.
Ready to unlock the power of connected care? Contact Arkenea’s medical device integration experts today to design a tailored solution that meets your clinical, technical, and compliance needs. Let’s transform healthcare delivery together.
